
Managing trainee in difficulty
Introduction
Supporting a trainee in difficulty can be extremely challenging, yet immensely rewarding.
This module explores the types of difficulty trainees may experience and considers a range of potential intervention strategies that may be adopted by supervisors to ensure the continuation of a positive training experience for all trainees.
We use the term “trainer” generically, unless there are particular roles for specified members of the training team. Throughout the module there is a focus on those areas where educational insights and expertise can have an important impact – in other words, where you can make a real difference.
It is anticipated that by the end of this module you should have a clearer sense of the types of difficulty trainees may experience, what the underlying causes may be and the strategic interventions you may be able to make (including seeking help from others in the team) to manage and support these trainees.
Before you start
Before you start the module we recommend that you spend a few minutes thinking about the following points and noting down some of your thoughts.
Thinking points
Consider your own training and identify any difficulties you faced.
- What types of intervention did you find helpful or wish had been available to you?
Consider your own experience of supporting trainees.
- What kinds of ‘challenge’ do they face in their training years?
- What difficulties have you encountered when supervising trainees?
A summary of roles and responsibilities for those involved in training
| Trainee | Holds a contractual relationship with their employer and is therefore subject to local and national terms and conditions of employment. All trainees hold an NCHD contract. |
| HSE or Voluntary Hospital | Is responsible for management of performance and disciplinary matters yet, should keep the College advised of any issues arising. Colleagues in human resources and occupational health may also be involved Educational and clinical supervisors are likely to be involved in the identification, management and support of the trainee in difficulty. Those with more senior Training roles such as the Specialty Training Programme Director (TPD) may become involved, depending on the nature and severity of the difficulties faced |
| Royal College of Surgeons in Ireland RCSI | Is responsible for all surgeons in training and problems that arise which prevent normal progressions. They can offer a range of support to trainees in difficulty and their supervisors. They also quality manage training programmes and should address any concerns that arise |
| Medical Council of Ireland IMC | May be involved where there are concerns around fitness to practise. |
Supporting a trainee in difficulty can be challenging: the old adage of a ‘problem shared is a problem halved’ holds true. As a trainer it is important to access the support and guidance of colleagues with more senior training roles and responsibilities within your workplace, and also within the RCSIs, who hold a wealth of knowledge on how to best support trainees.
Different Types of Difficulty
In considering ways to best support a trainee who is experiencing difficulties, it is important to distinguish between three ‘categories of difficulty’.
The emphasis here is the trainee in difficulty, that is, a trainee who is failing to make satisfactory progress overall or has areas of specific difficulty with their training.
However, as a trainer, you are likely to come across trainees with difficulties of a transient, more personal nature, who for a certain period of time need particular support. Finally, you may also come across trainees who you and others find ‘difficult’ (the so-called ‘difficult trainee’) because of conduct issues.
Distinguishing between these different types of difficulty can be seen as a triage process, involving looking for ‘signs and symptoms’ and gathering ‘case’ information, before formulating a diagnosis of difficulty and subsequent management plan.
As a trainer, it is often easier to manage the first two situations than the third, and it is helpful to distinguish problems that arise from current circumstances (see box below) from problems that are related specifically to the personality and behaviour patterns of a trainee.
Common circumstantial problems for trainees
- educational challenges, exams, revision
- anxiety concerning career decisions
- pressure of work, lack of team support
- unfamiliarity, inexperience
- changes in team dynamics
- personal health problems
- sickness within the family
- personal relationship difficulties
- cultural isolation, culture shock (e.g. overseas graduates)
- domestic responsibilities or pressures
It is helpful to apply a triage process to the doctor in difficulty, in a similar way to other clinical problems, by considering the history, the presenting problem, and the relevant social and employment context.
Thinking points
Think of a trainee in difficulty you have supervised in the past.
- How were you alerted to the possible difficulties the trainee had?
- Was it an isolated instance or were you aware of a repeating pattern of concerns?
- What information did you need to help the trainee (e.g. observations, workplace-based assessments, reported concerns from others in the team)?
Trainees in Difficulty Situations
Trainees with personal conduct and performance issues are likely to be in the minority but often occupy a considerable amount of supervisor time and energy.
Trainees are employees and, as such, are expected to demonstrate appropriate professional behaviours with patients, families and colleagues.
Behavioural issues may be brought to your attention, and it is important to be fully aware of the IMC Guide to Professional conduct and ethics which applies to all doctors including those in training. Where there are potential infringements of the IMC’s guidance, consider the relative seriousness of the problem, and if in any doubt consult with the appropriate colleague(s).
In practical terms, it is important to be clear about whether there is an issue of improper personal conduct, which would be subject to employment regulations, or an issue of poor professional performance.
A useful distinction between these two categories is that matters of personal conduct – such as absence without leave, theft of hospital property, bullying or sexual harassment – will normally apply equally to any employee. If a trainee’s behaviour or conduct has been questioned, then it is appropriate to agree with the Training Programme Director or Dean of Post Graduate Training on how any allegations of concern should be investigated in accordance with local human resources policy. Conduct issues with serious implications for the future professional work of the trainee should also be reported to the College after investigation is completed. Actions should also respect national policies, IMC regulations and any obligations under law.
As a trainer, you should ensure that accurate, contemporaneous, dated and signed records of feedback, the ISCP tool would be best used for this purpose, so all training records are in the one place
Recognising Signs and Symptoms
Paice (2006) identifies seven key early warning signs of a trainee in difficulty, characterised in terms of observed behavioural patterns. These patterns may relate to behavioural problems per se, or reflect underlying educational or personal difficulties.
Seven key early warning signs
- The ‘disappearing act’: not answering bleeps; disappearing between clinic and ward; lateness; frequent sick leave.
- Low work rate: slowness in doing procedures, clerking patients, dictating letters, making decisions; arriving early, leaving late and still not achieving a reasonable workload.
- ‘Ward rage’: bursts of temper; shouting matches; real or imagined slights.
- Rigidity: poor tolerance of ambiguity; inability to compromise; difficulty prioritising; inappropriate ‘whistle blowing’.
- ‘Bypass syndrome’: junior colleagues or nurses find ways to avoid seeking the doctor’s opinion or help.
- Career problems: difficulty with exams; uncertainty about career choice; disillusionment with medicine.
- Insight failure: rejection of constructive criticism; defensiveness; counter-challenge.
If you notice any of these warning signs in your own trainee, the first step is to identify an opportunity to share your concerns with the trainee, being careful to focus on observable behaviours rather than personal characteristics or traits.
An early conversation of this nature may rapidly identify the possible cause(s) of the trainee’s difficulty, which can then be dealt with immediately. Some trainees may readily disclose information to a supervisor who clearly indicates their willingness to listen and support. Others may have concerns about revealing information to those who they perceive to have power to influence their progression. You may wish to encourage those who are not immediately forthcoming to seek help elsewhere by labelling your concerns and suggesting they may wish to speak to others within the organisation, guiding them towards the appropriate personnel.
Trainees in Difficulty
Trainees in difficulty are those who are not making sufficient progress in training or who are experiencing difficulties with certain elements of training.
Trainees enter the workplace following years of intensive, formal education. A report commissioned by the GMC (Illing et al., 2008) shows that new graduates report feelings of un-preparedness for practice, of uncertainty about the roles and responsibilities they carry, and they may have very limited experience of hands-on care. In contrast, most doctors’ postgraduate learning is in the workplace, happening alongside service commitments and arising opportunistically. It is valuable to emphasise the point, since failure to progress educationally as a doctor is usually likely to relate to a failure in learning within the workplace.
Swanwick (2005) describes the role of the trainer as that of ‘structuring experiences, rather than transmitting knowledge’, which underlines the importance of the experiences themselves as the vehicle for learning, rather than the knowledge of the trainer. In ‘structuring experiences’ in this way, the educational supervisor not only makes learning opportunities in the workplace explicit, but also has the ability to modify the learning culture within the workplace.
Trainees in difficulty may need help in identifying the learning opportunities that arise in the workplace, and encouragement to value and seize the opportunities for learning they offer. Such trainees (particularly those who are felt to lack insight) may have reduced access to certain types of work as trainers have concerns about quality of care and so do not delegate certain aspects of work activity to them. Limiting trainees’ learning opportunities may compound the difficulties the trainees are experiencing. Trainers can help by identifying ways of enabling learning, making learning opportunities explicit, and using briefing and debriefing to help the trainee appreciate the value of these opportunities. Trainees in difficulty need more experience rather than less, if they are to make progress. As a Trainer, your role in ‘safety netting’ becomes increasingly important.
Creating a learning environment
Trainees in difficulty will undoubtedly benefit from targeted and effective clinical and educational supervision based on assessment for learning principles and a personalised curriculum for workplace-based learning. However, as with all trainees, the need to create a ‘safe’ learning environment will be as important.
Trainees who face difficulties may well struggle to achieve what they are capable of achieving. The need to attend to the emotional dimensions of learning is evident in these situations. Learning in the workplace is about learning with and from others. Most of us can remember at different times how we may have tiptoed around the workplace, trying to second guess what was expected of us as the newcomer. Trainees face these challenges on a regular basis. Turnbull notes that:
As organisational members, we learn to collaborate, influence, negotiate, motivate, and achieve results through our interaction with others, all of which can be highly charged with emotion (Turnbull, 2000, p. 3).
It is important to ensure that the workplace enables trainees to feel that they are part of a team. This involves all members of the healthcare and support team conveying positive messages to trainees so that the workplace culture and support mechanisms welcome, involve and value the regular influx of new trainees. Trainees in difficulty may need longer than most to recognise and adopt tacit rules of behaviour, which may include learning what are ‘acceptable’ displays of emotion in each setting.
As Trainers it would be worth noting the significance of positive emotions in educational experiences and address any approaches to learning that exploit fear and humiliation as key ‘motivators’. On this issue there is general agreement: negative approaches to education have little evidence of their effectiveness. For example, Moore and Kuol (2007) analysed students’ recollections of excellent teaching and observed that these included interest, intense positive affect, humour, fun, enjoyment, enthusiasm, commitment, dedication and compassion. Significantly, the authors determined that a teacher’s attributes were invoked more frequently than their actions by students, as they recalled positive learning experiences. They were led to conclude that ‘who a teacher is with their students’ was more relevant in the recollection of good learning experiences than ‘what a teacher does with his/her subject’ (2007). Reflect on what this insight might tell you about the trainee in difficulty, in relation to their trainer.
Interventions and Strategies
The introduction of a structured training curriculum and workplace-based assessments enable Trainers to bring together a range of helpful ‘diagnostic data’ and indicate the type(s) of learning experience trainees may need to overcome difficulties. The primary goal is to identify the nature and extent of the difficulties they face.
Personal development plans, if used effectively, can help trainees recognise gaps in their experience, skills or knowledge and be used to set goals for future development. The educational supervisor can assist the trainee in difficulty to identify the underdeveloped areas in their learning portfolio while encouraging the trainee to take the lead in this process. Facilitating ‘developmental conversations’ which highlight the possibilities for further personal growth and understanding through a consideration of new ideas and ways of addressing areas of difficulty are vital.
Workplace-based assessments can be extremely helpful. These tools provide a means of capturing early warning signs of the trainee in difficulty. Multi-source feedback is particularly useful, with careful interpretation of data to identify profiles of underperformance. Trainees who consistently over-rate their own performance may be a particular cause for concern.
Observation of a trainee’s practice in the workplace, either formally or informally, is particularly useful in contextualising reported behaviour provided by others in the team. It may facilitate the possibility of distinguishing between occasional and systemic difficulty on the part of the trainee in a particular assessment. Thus direct observation of, say, a consenting procedure by a trainee, may simultaneously give insight into communication skills and technical understanding. The latter may be a small weakness in knowledge base, the former an underlying behavioural characteristic.
Thinking points
The Trainer is in a position to have a direct and positive impact on the trainee’s programme of learning. For the trainee in difficulty consider the following.
- What information do I need to ensure an accurate ‘training needs analysis’ and an appropriate development plan?
- Do workplace-based assessments indicate consistent areas of underperformance?
- What information might I gain from directly observing the trainee with patients or working with other team members?
- Which tools and strategies might I use to help the trainee to internalise appropriate learning objectives and to engage them in the process of addressing development needs?
Common areas of difficulty and how to approach them
| Area of difficulty | Approaches to identification | Possible educational interventions |
| Practical skills/procedures | Assessed or observed practice Feedback from colleagues Errors reported | Specific feedback and guidance Purposeful observation of those skilled in the procedure Simulation Close supervision and repeated opportunities to practise |
| Communication skills | Mini-Cex, multi-source feedback, observation Feedback from patients, carers, colleagues | Specific feedback and guidance Video recording with self-review Formal training |
| Clinical reasoning | Case-based discussion, clinical teaching (on rounds, in clinic, etc.) Over-reliance on investigations Diagnostic errors | Developing knowledge base Use socratic questioning techniques in supervision Data interpretation (results of investigations, etc.) Informal case-based discussion with a focus on rationale for choices made, along with consideration of alternative options (diagnosis, investigations, management) Increased clinical exposure (clerking, history taking) and requirement to present cases |
| Insight into performance | Multi-source feedback Self-ratings Evidence in feedback (capacity to self-evaluate) and supervision sessions | Encourage independent review of performance in all feedback sessions Encourage trainee to self-rate assessments before sharing your ratings – then discuss difference in perceptions (with evidence to back up) Develop competence through increased opportunities to practise (being able to recognise a competent performance is a key step to developing insight) Regular feedback, with specific supporting examples and guidance |
| Team working | Multi-source feedback, feedback from colleagues and observed behaviour | Shadowing team members to develop awareness of their roles and contributions Case-based discussion to explore who else to involve in patient management (and why) Specific feedback, guidance and goal setting |
Trainees with Difficulties
All of us are likely to face difficulties at some points in our careers and trainees are no exception. Typical difficulties trainees may face include difficulties with their own health, with (personal) relationships or with career-related concerns.
The Trainer’ role with the trainee with difficulties may be limited to the recognition of early warning signs and ‘referral’ to colleagues able to provide specific and/or specialist advice or support. It is really important to maintain supervisory boundaries, and while your medical knowledge and counselling skills may be of value, you must remember you are not your trainees’ doctor or their counsellor.
This section of the module synthesises the types of difficulty trainees may face, their implications and the management and support mechanisms available.
Health issues
Physical and/or mental health issues, e.g. diabetes, depression or epilepsy, may arise during training or be of a long-standing nature, disclosed to an employer but not necessarily to individual Trainers. There may be a need for some staff to be aware of certain health issues in order to handle episodes such as potential loss of awareness in an appropriate manner. More subtle health issues may be difficult to discern, and it is helpful to seek input from a range of sources – such as senior nursing staff, clerical and secretarial staff, in addition to other medical staff in contact with the individual – all of whom may have differing perspectives and insights that will help to build a rounded and balanced picture. Some additional short-term support, changes to duties or time out may be sufficient for the trainee to regain health.
Mental health issues and alcohol and drug misuse are more often not disclosed, but where there is cause for concern and patient care or safety may be compromised, advice should be sought from occupational health and human resources (HR) immediately, as trainees are also employees with service commitments. Significant health difficulties may raise issues around fitness to practice. Whatever the health issues faced, it is important to ensure that trainees are treated fairly.
Personal issues
Trainees may experience difficulties with personal relationships or may have carer responsibilities that impact on their ability to fully engage with their training at times. Where these difficulties are sustained and having an impact on their training or their service commitments, you may wish to involve other members of the team in identifying strategies to support the trainee.
Colleagues in HR will be able to advise the trainee of rights in relation to carer or parental leave, for example. Where the disruption is significant, you may need to involve the TPD in identifying options for time out, flexible training or an extension to the training period.
Stress and Burnout
Doctors are exposed constantly to risks, including stress, alienation, over-involvement, automatic behaviour, and burnout… The medical profession has until now been in the paradoxical position of needing as much… [support] …as any other group of clinicians (if not more), but generally getting less (Launer, 2006, p. 24).
One of the greatest challenges is to create a culture where difficulties are accepted as part and parcel of professional life. The social implications of the pursuit of a medical career, as well as the major cognitive challenges, need to be considered. Firth-Cozens (2003) emphasises the significant levels of stress among junior doctors – with 28% showing above threshold levels of stress, compared to 18% in the general working population. Differences in perceptions of and responses to stressful circumstances may well be indicative of personality predispositions. For example, McManus et al. (2004) reported a large-scale longitudinal cohort study of UK medical students and determined that personality traits, identifiable at the time of application to medical school, are strong predictors of subsequent job satisfaction and of the perceived supportiveness of the working environment. These traits include neuroticism, which shows a strong predictive effect for stress, and surface learning style, which is associated with a later surface-disorganised approach to work, and tends to predict expressions of high perceived workload. In contrast, the trait of ‘agreeableness’ is associated with later perceptions of supportive work environments. They suggest therefore that:
stress is not a characteristic of jobs but of doctors, different doctors in the same job being no more similar in their stress and burnout than different doctors in different jobs (McManus et al., 2004, p. 9).
It is not difficult to understand that a welter of negative feelings in an overworked, isolated, possibly frightened doctor may lead to disinterest in learning, and to feelings of estrangement from the professional community, as suggested by the following description of burnout.
What started out as important, meaningful and challenging work, becomes unpleasant, unfulfilling and meaningless. Energy turns into exhaustion, involvement turns into cynicism, and efficacy turns into ineffectiveness (Maslach et al., 2001).
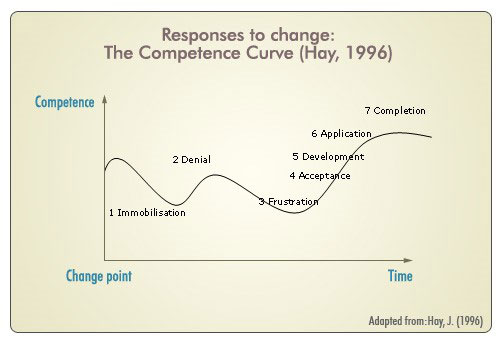
McKimm (2009) notes the importance of being sensitive to the support needs arising during periods of change and transition and draws on Hay’s model of the Competence Curve (see figure) to highlight the possible responses trainees may have to personal change and stressors, which may compromise their competence for a period of time. As a supervisor, it is important to be alert to signs of difficulty and ready to provide specific targeted input as the trainee moves into stages of acceptance and development. McKimm suggests routinely building in 10 minutes of ‘talk time’ at the beginning or end of a supervision session, where the trainee is invited to talk about any personal issues that may be causing concern. This approach provides the trainee with permission to raise issues with you and acknowledges the interplay between ‘work’ and ‘life’.
Thinking points
Think about trainees who seem to struggle in your specialty or workplace.
- What characteristics do they seem to have in common?
- What strategies might you be able to put in place to support their transition?
- What interventions or strategies could you put in place to increase a sense of supportive work environment?
Summary
The effective management and support of a trainee in difficulty is complex and approaches adopted will vary depending on the nature of the difficulties faced by the trainee and your role in training. However, some general principles are relevant for all.
- Seek to create an open, trusting relationship with all trainees, where the interplay between work and life is acknowledged and respected.
- Know your structures and use them well. A trainee in difficulty is likely to require advice and guidance from a range of people, and, as their Trainer, so will you.
- Keep contemporaneous records of all encounters with the trainee in accordance with HSE and RCSI guidelines.
- Use workplace-based assessments diagnostically. It is vital that you are explicit about labelling all causes for concern and that these are recorded.
- Set realistic goals for improvement, monitor these and record outcomes. The importance of ensuring clear feedback, based on observable behaviours and with specific suggestions for improvement cannot be overstated here.
- Remember that trainees in difficulty are also employees in difficulty, who may put patient care or safety at risk. Involve appropriate colleagues with specialist skills within your organisation and the RCSI at an early stage.
- Don’t underestimate the power of regular ‘developmental conversations’.
Useful Links;
Practitioner Health – Confidential Help for Medical Practitioners https://practitionerhealth.ie/
Psychological Society of Ireland https://www.psychologicalsociety.ie/
