Knee Replacement
There are man implants. Depending on the type and severity of the disease, they may be
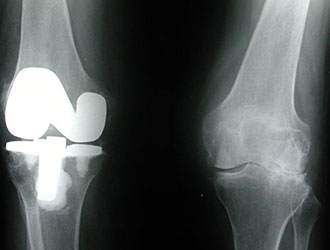
- Total Condylar Prostheses - The most commonly used and described below. The articular surface of the tibia and femur is replaced and the patello-femoral joint resurfaced. They are made of cobalt, chrome or titanium alloys and an ultra high molecular weight polyethylene tibial bearing surface. They may be cemented or press fitted allowing bone growth into a roughened metal surface.
- Unicompartmental - The most common indication is for a varus knee with medial osteoarthritis. The other compartment and ligaments must be intact.
Pre-operative Preparation
Includes cross matching of blood and prophylactic antibiotics. Adequate radiology to allow pre-operative planning. The mechanical axis should pass through the centre of the knee and bone cuts of the femur and tibia should bring the transverse axis of the knee parallel to the ground.
Anaesthesia
General or spinal.A tourniquet is applied following exsanguination of the limb.
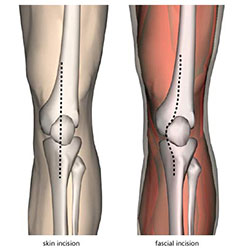
Incision
A vertical midline incision is made from 4 inches above the patella to below the tibial tuberosity.
Procedure
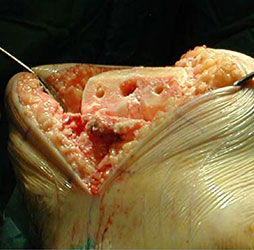
- The dissection is continued and the prepatellar bursa is divided to expose the rectus femoris muscle, patella, infra-patellar tendon and tibial tuberosity.
- The medial capsule of the knee joint is incised up to the rectus femoris tendon, around the medial patella and onto the lower margin of the tibial tuberosity.
- The knee joint is opened and the patella is dislocated laterally to provide good exposure of the articular surfaces.
- The joint capsule is excised and a synovectomy performed, if necessary.
- Femoral and tibial cuts are made on the bony surfaces and trial implants are inserted to assess the initial fits.
- Tissue releases are carried out as required and correct patello-femoral tracking is established.
- After final preparation the femoral and tibial components are put in place and the knee joint reduced.
Closure and Drainage
In layers, with firm closure of the medial arthrotomy, over a closed suction drain.
Postoperative Management
Varies with surgeon but might include:
- Quadriceps and hamstring isometric physiotherapy from day 1.
- Drain removal on day 2.
- After wound inspection on the day 5, the knee is mobilised, achieving 70-80° flexion and partial weight bearing prior to discharge.
Main Postoperative Complications
Those associated with joint replacement operations - infection, venous thromboembolism and aseptic loosening. Those specific to knee replacement - persistent patello-femoral maltracking and peroneal nerve injury.