Skin Grafting
Skin grafts are used to cover skin defects. The thicker the graft, the better the cosmesis. The recipient site must have a good blood supply or else the graft has to come with its own blood supply as in a flap graft. Free skin grafts are descrived here and may be:
- Split skin suitable for large areas and takes well especially on healthy granulation tissue.
- Full thickness (Wolfe) gives better cosmesis and wear, but cannot be used for large areas or on granulation tissue. They are ideal for facial defects or finger tip injuries.
- Grafts will not take on necrotic or infected tissue. Any vascularised bed can be grafted but exposed bone, tendon and fat needs to granulate before receiving a split-skin graft.
Anaesthesia
General, local or regional, depending on the site and size of the donor and recipient areas.
Split-Skin
- The donor and recipient areas are prepared and draped.
- The harvested skin donor skin must be adequate to cover the recipient defect. The inside of the thigh is commonly used. Re-harvesting from a site can be performed after 20 days of re-epithelialisation but should be restricted to two thin re-harvests.
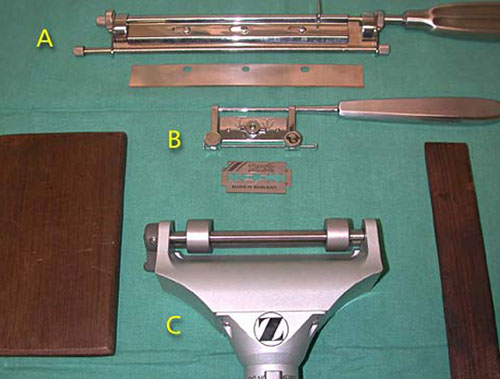
- Dermatomes are used to take split skin grafts. They have sharp blades and the most common include variations of the , (a) Humbly knife, (b) the Silver, or (c) mechanical dermatomes powered by electricity or compressed air.
- The blade on a skin grafting knife is adjusted to the appropriate gap to allow excision of split skin to the thickness required, varying from thin, 8-15jm (Thiersch) to thick, 20-30jm.
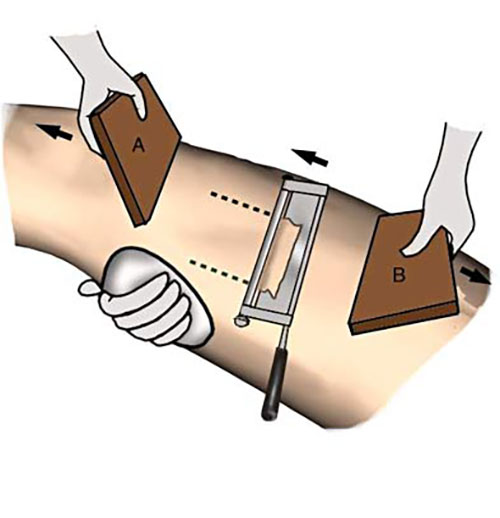
- The donor skin is stretched by an assistant and the graft taken with smooth slicing strokes as shown using a Humby knife on the inside of the thigh.

- The skin is immediately placed onto paraffin gauze, with the under, shiny side facing upwards
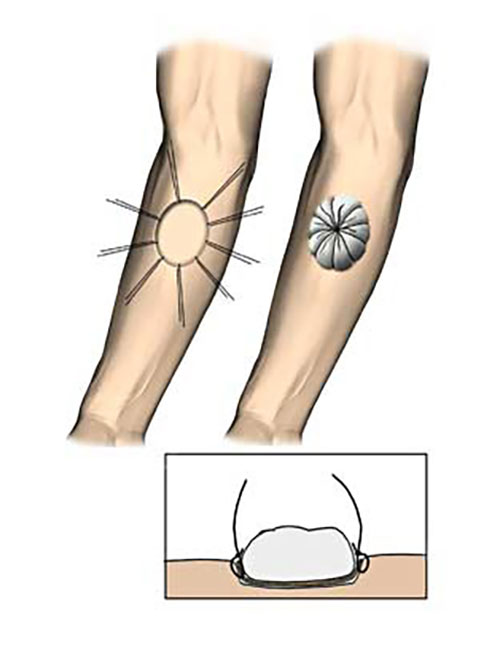
- A series of perforations or stabs aids graft adhesion by preventing fluid accumulating and separating the graft from the underlying tissues.
- The graft is placed on the recipient area, which has been prepared by debridement or abrasion of any granulation tissue, and trimmed into shape with scissors.
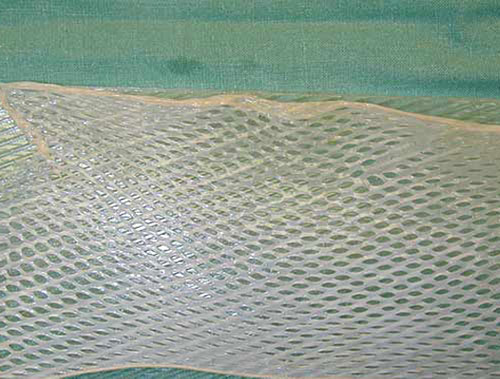
- Meshing of the graft increases the area which can be covered from a given donor site, as well as increasing the take rate and confirmability of a graft.

.
- The graft is secured with sutures, clips or glue.
- It is then firmly dressed under even pressure to ensure stable contact with the underlying tissues. Tie over dressings using flavine soaked wool are useful for concave wounds.

- The donor area is dressed with hydrogel, plastic film, or calcium alginate to provide a moist environment.

.

Full thickness
- The recipient area is carefully prepated with complete haemostasis.

An exact pattern of the defect is made with paper or foil.
- A non-hairy donor is chosen; common sites include the skin behind the ear, the supraclavicular area, or the front of the forearm.

- The pattern is laid on the donor site, and an exact area of skin is excused and prepared for grafting by removal of all subcutaneous fat with a sharp scissors.

- The graft is then placed on the defect and sutured to the margins without tensions.
It may then be secured and dressed with a tie-over dressing.
Finally, the donor site is closed primarily with sutures.</p.
Main Postoperative Complications
These are failure of the graft to vascularise with resultant necrosis and infection.
Related Technique
Other techniques used to obtain skin cover include:
- Various local flaps - advancement, transposition and Z-plasties.
- Random pattern flaps such as the cross-finger flap.
- Fascio-cutaneous flaps that come with their specific arteriovenous system and may include other tissues (compound), such as muscle, e.g. the latissimus dorsi flap used for reconstruction after mastectomy.
- Free tissue transfer flaps are often compound and require microvascular anastomosis to suitable vessels at the recipient site.
- Tissue expansion, with subcutaneous silicone expanders over several weeks, can be used to provide a local flap.
