Common Fracture Surgery
Remember to treat the patient as a whole, taking consideration of first aid measures, how the patient is to be transported as well as the treatment of shock, blood loss and associated injuries. Fracture treatment will also take cognisance of whether it is open or closed, the amount of soft tissue injury and the time since the injury.
Treatment of Closed Fractures
The main principle include:
- Reduction of the fracture
- Holding the reduction
- Rehabilitation
Reduction
Is unnecessary when there is minimal displacement, when displacement does not matter 9e.g. the clavicle), or when it is unlikely to succeed (e.g. compression of the spine).Is closed, for example, in a simple Colles fracture. Under anaesthesia and muscle relaxation, traction is applied in the line of the bone to distract the fragments that are then aligned by reversing the direction of the original force.
This is used for most minimally displaced fractures that are stable after rediction and fractures in children.Is open, when closed reduction fails, when a fracture into a joint needs accurate positioning, or for traction fractures when the fragments are held apart.
Holding the Reduction
May be achieved by:
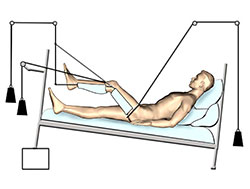
a) Continuois Traction
Is now rarely used except for short period prior to internal fixation, because it immobilises the patient and prolongs hospital stay.
Is applied to the limb distal to the fracture as skin or skeletal traction but may also be achieved by gravity (e.g. for a fracture humerus).
Traction must always be opposed by counter-traction which may be fixed, as with a Thomas splint which abuts against the root of the limb.
This can be counterbalanced by the patient's own weight as in balanced traction. (e.g. skeletal tration used for thigh or hip injuries requires the placement of a Steinmann pin behind the tibial tubercle.).
Complications include circulation compromise, peroneal nerve injury and compartment syndrome.
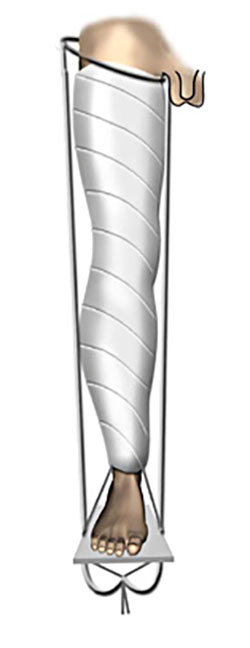
b) Splintage with a Plaster Cast
- Is safe and is commonly used for distal limb and children's fractures and allows early discharge.
- After reduction, place a stockinette over the limb and protect boney prominences with wool.
- Apply the wet plaster, moist and in layers, while smoothing each layer away from the boney points. Maintaine reduction while the cast is setting.
- If the fracture is recent, the plaster is left as a backslab or split to allow for swelling. A check X-ray is performed.
While Plaster of Paris is used initially in th treatment of fractures (split or backslab) and is better for moulding, it is not more common to use casts made of fiberglass impregnated frabric with ployurethane resin for the definitive cast because it is lighter, stronger, sets quicker and is water resistant.
Complications inclide a tight cast with vascular compression and pressure sores.
c) Functional Bracing
Segments of plaster cast are applied over the shafts of long bones, usually the femur and tibia, and united by a hinge which allows joint movement in one plane. It is usually applied after early union of the fracture at 4-6 weeks but there is an increased risk of malunion.
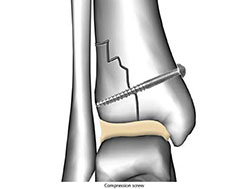
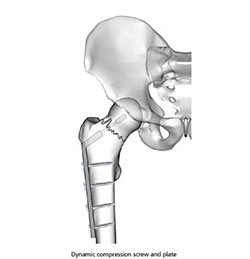
d) Internal Fixation
By holding the fracture together this allows early movement, avoiding stiffness and oedema. It must provide sufficient stability to maintain length, alignment and rotation. Rigid fixation aims to provide direct healing which is achieved by interfragmentary compression. It requires absolute anatomical reduction and is used for articular and simple fractures, using lag screws (a) and plates (b).
Non-rigid fixation allows the fracture to stabilise by natural callus healing as seen with intramendullary nails (and external fixators). There are many methods of internal fixation which may often be used in combination. Some examples are shown.
Complicatons include non-union, infection, implant failure and refracture.
e) External Fixation
Transfixing screws or tension wires passed through the bone above and below the fracture and attached to an external frame holds the fracture.
It is commonly used for the tibia and pelvis, but also for the femur, humerus, lower radius and bones of the hand.
It is useful for severe comminuted or unstable fractures or when there is a lot of soft tissue injury or infection.
There are many devices and the system of hoops and tenison wires devised by ilizarov (1992) is particularily versatile.
Complications include overdistraction, delayed healing and pin-track infection.
Rehabilitation
Has many aspects but would include:
- Prevention of oedema
- Elevation
- Active exercise
- Assisted movement
- Encouragin functional activity
- Treatment of Open Fractures
- After the general assessment and resuscitation, ascertain the nature of the wound, and the state of the surrounding skin (an open fracture may vary from a small skin puncture to an extensive high velocity injury), the local circulation and any nerve injury. The incidence of wound infection correlates with degree of injury and the control of sepsis is paramount.
- Early, the wound is inspected under general anaesthetic, lavaged with saline, cleaned and debrided of dead tissue, especially muscle.
- Wounds are generally left open and packed or dressed, unless they are very small and clean.
- The safest method of fracture stabilisation is by external fixation but a widely split plaster can also be used.A fracture should be an arterial repair is performed.
- Aftercare includes the continuation of antibiotics, wound inspection, skin grafting if necessary, and the on-going management of the fracture and any joint injury.