Thorascopic Sympathectomy
Hyperhidrosis is the only absolute indication. It gives good early results in Raynaud's disease but symptoms return in 6-12 months. It may help in some circumstances in cervical rib syndrome, post-traumatic pain & causalgia. Thoracoscopic cervical sympathectomy, described here, is now the standard operation with open techniques, such as the transaxillary or supraclavicular approaches, rarely being required. Because the upper thoracic ganglia are ablated it should be correctly called a 'thoracic sympathectomy'.'
Anaesthesia
General with a double-lumen endotracheal tube.
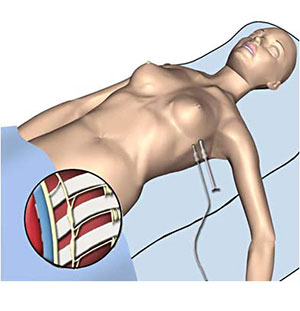
Position
Supine with both arms abducted to 60°.
Procedure
- Make a small incision through 3rd intercostal space in midaxillary line. This is used to place a finger in order to guide the placement of a 10mm port into the pleura.
- Under laparoscopic view, the ipsilateral lung is deflated by the anaesthetist.
- Place a 5mm working port into the 4th or 5th intercostal space in the anterior axillary line.
- Push the apex of the lung downwards to display the costo-vertebral angle.
- Follow the ribs medially until the sympathetic ganglia & chain are seen over the necks of the ribs as a white glistening structure.
- Ablate the fifth ganglion if axillary hyperhidosis is present.
- On completion re-inflate the lung under laparoscopic view.
Intra-operative Problem
The azygos vein lies close to the sympathetic chain on the right side & requires careful mobilisation to expose the sympathetic chain.
Closure
The port sites are closed routinely.
Postoperative Management
A chest X-ray in the recovery area is performed to check for residual pneumothorax.
Main Postoperative Complications
Include Horner's syndrome if T1 is damaged. Also, compensatory hyperhidrosis.